Family Practice Physician, Full Health Primary Care-UPMC, Pittsburgh, Pennsylvania
Implementation of a 4th Trimester Care Model to Improve Maternal and Child Health: Designated OB Care Coordinators Greatly Improve Return for Postpartum Care
Authors:
Marielle Williamson-Rea, DO; Stephanie Ballard, PharmD, BCPS; Rowena Pingul-Ravano, MD; Maggie Judge, RN, BSN, LCCE, CLC; Stacy Bartlett, MD; Carolyn Kirby, MPH; Lisa Schlar, MD
Introduction:
Historically, postpartum (PP) care was provided at a single visit around 6 weeks PP. In 2018, ACOG updated guidance of care to mother/birthing persons and baby “dyads,” recommending PP provider contact within the first 3 weeks, and a comprehensive PP visit no later than 12 weeks. This project is an implementation of this external mandate to bring the dyad back to the clinic sooner after birth, and to identify and address dyad health concerns in the late prenatal and early PP period, to ultimately reduce dyad morbidity and mortality.
Methods:
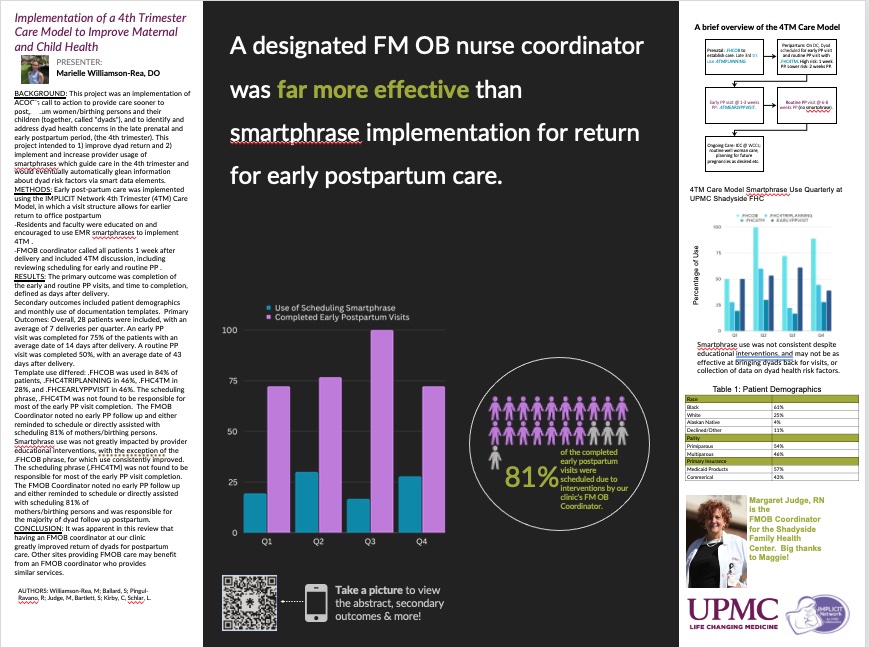
Patients included were those who delivered between February 2022 through January 2023, who received prenatal care primarily at the Shadyside FHC. Patients with prenatal care fully transferred to maternal fetal medicine service were excluded. Early PP care was implemented using the 4TM Care Model. Four documentation templates (“smartphrases”) were created to facilitate scheduling and care organization. Providers were educated on smartphrase use and reminded of use though lectures, emails, and a bulletin board. A nurse FMOB coordinator called all patients 1 week after delivery and included 4TM discussion, including reviewing scheduling for early and routine PP.
Results:
Overall, 28 patients were included, with an average of 7 deliveries per quarter. Early PP visits were completed for 75% and routine PP visits were completed for 50% of patients included. Template use differed: overall, use of smartphrases was low despite provider educational interventions. The scheduling phrase, FHC4TM was not found to be responsible for most of the early PP visit completion. The FMOB Coordinator noted no early PP follow up and either reminded to schedule or directly assisted with scheduling 81% of mothers/birthing persons. Demographic data was also reviewed.
Conclusions:
It was anticipated that resident, faculty, and staff education, easy access to resources, and frequent reminders of the care model would improve implementation of the care model, measured as return for PP visits and appropriate use of EMR smartphrases. However, despite several interventions to encourage use, the implementation of smartphrases was not overall successful at our clinic. While some dyads returned for PP care due to scheduling by smartphrase use, the majority returned because of FMOB coordinator intervention. This review was also able to identify via demographic data collection many pregnancy or PP complications in the study population, highlighting the necessity of improved PP care