Title: Screening for Adverse Childhood Experiences (ACEs)
Authors: Katayon Kochakzadeh, DO; Scott Brown, DO; Alissa Cohen, DO, MS, DipABLM; Lori Stiefel, MD; Jacqueline Weaver-Agostoni, DO, MPH, DipABLM, FACOFP
Background:
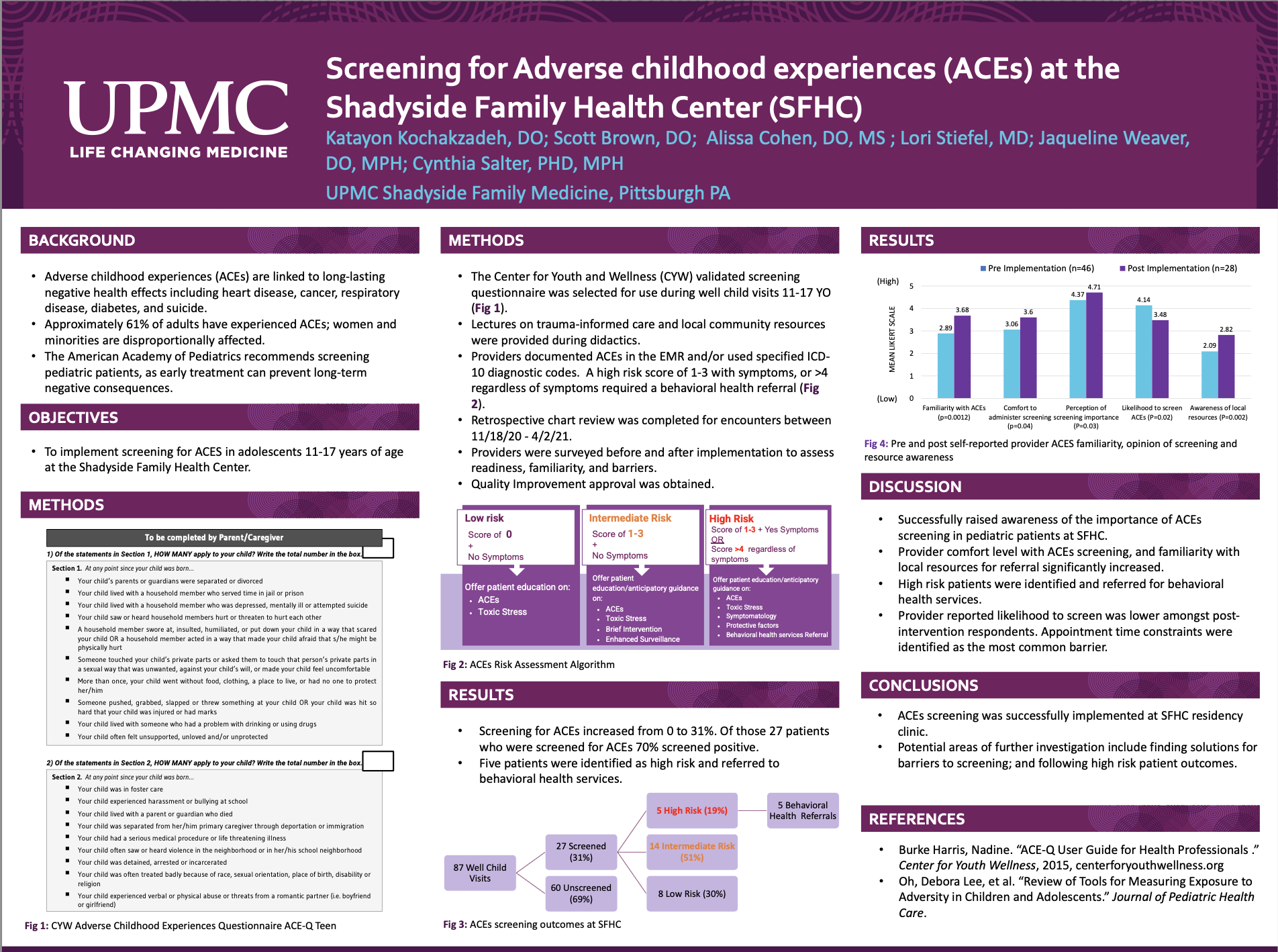
ACEs are traumatic childhood events that have been linked to long-lasting negative health effects. Approximately 61% of adults have experienced ACEs. The American Academy of Pediatrics recommends screening pediatric patients, as early treatment can prevent long-term negative consequences. Prior to this project, screening was not standard of care at the Shadyside Family Health Center (SFHC). This project led to initiation of ACEs screening, measuring completion rates, and referrals for intervention.
Methods:
The Center for Youth and Wellness (CYW) validated screening questionnaire was selected for use. Providers were surveyed before and after screening implementation to assess their readiness, familiarity, and barriers. They also received lectures on trauma-informed care and local community resources. The screening tool was provided to patients aged 11-17 years during well-child visits. Providers documented ACEs in the EMR and/or used specified ICD-10 diagnostic codes. The questionnaire was scanned into the patient chart. A retrospective chart review was completed for encounters between November 18, 2020-April 2, 2021. Quality Improvement approval was obtained.
Results:
Of 87 well-child visits completed, 27 were screened for ACEs (31%); 19 (70%) of those had a positive score, and 5 patients were referred to community resources. The results show that following the implementation of this study and trauma-informed care lecture, 64% percent of providers felt more comfortable screening for ACEs compared to 28% before the intervention. 61% of providers reported time constraints as the largest barrier to screening.
Conclusions:
This intervention increased screening rates at the Shadyside Family Health Center. It is crucial to screen and refer children to resources in order to prevent long term sequela of chronic disease, and this can be done at a residency clinic. However, follow-up discussions and education are needed to further increase provider comfort and find solutions for barriers to screening as well as effective referral for treatment.